Developing AI responsibly to help patients get treatment sooner


This story is part of the Forward happens here series.
Dr. Raymond Ng is using AI to identify crucial data in the health-care system, streamlining processes for the benefit of both patients and staff
Have you ever gone to the doctor and struggled to recall your own medical history? Perhaps it was the name of a medication prescribed by a previous doctor, the results from a specialist, or treatments you had years ago.
Most people don’t have comprehensive records of their own health, and their doctors don’t either. Patient records are often scattered among different doctors, specialists and across health-care systems, says Dr. Raymond Ng, a University of British Columbia computer science professor and Canada Research Chair in Data Science and Analytics.
“We have very deep health data that actually exists, but it’s buried in filing cabinets,” says Dr. Ng. “Imagine if we could extract that and consolidate it. So the next time when you have a problem and you see a physician, they would have a summary of all the key findings about your health. They could do a much more comprehensive diagnosis rather than just looking at a particular test that you did, for example, four weeks ago.”
That’s one way that artificial intelligence could be used to benefit our health-care system, says Dr. Ng, who is also Director of UBC’s Data Science Institute. Dr. Ng believes there is huge potential for AI to read documents and extract key data, speeding up the path to treatment, streamlining processes, triaging patients and expediting urgent cases. The key is to do it in a way that truly helps both patients and front-line workers, builds in safeguards around privacy and ensures that humans, not AI, make crucial health decisions.
Speeding up the path from diagnosis to treatment
Dr. Ng and his team study how to use natural language processing (NLP) to read and summarize data in health-care settings. “Modern medical research can create massive data sets,” explains Dr. Ng. “But without a way of sorting through all of that data, it isn’t useful for learning about, diagnosing or treating disease.”
Health-care providers diagnose breast cancer, for example, through a progressive series of mammogram, ultrasound and biopsy screenings. Each step results in a report that must be written, read and passed on to another provider and back to the family doctor. With a diagnosis, the family doctor then refers the patient to an oncologist at BC Cancer, who recommends a treatment plan. It can take up to six months for a patient whose report shows the markers of Triple Negative (aggressive) breast cancer to be referred to a chemotherapy oncologist at BC Cancer to start treatment.
But what if AI could identify and expedite serious cases early on?
Dr. Ng’s team is working with BC Cancer to develop a better system. “Our proposal is that the NLP could identify pathology reports with Triple Negative biomarkers and bring them to the attention of BC Cancer staff,” Dr. Ng explains. “The next day, staff can pull the report, confirm the diagnosis and contact the patient to discuss a treatment plan, such as starting chemotherapy.”
This would skip the wait for referrals, fast-tracking the most urgent cases to the attention of the person who can make a diagnosis. Such AI-assisted triaging could save lives. “Research has shown that every four weeks of delaying chemotherapy has a quantifiable negative effect on long-term survival rates.”
Dr. Ng emphasizes that AI would not make automated decisions. “The pathologists already identified crucial information in their report,” he says. “We just need somebody to assess it and make a diagnosis. If NLP could read it and fast-track it to the chemotherapy coordinator, it could save a lot of time in the process without losing the quality of the decision.”


“One of the reasons we’re so successful is that from day one, we’ve co-designed with front-line workers.”
– Dr. Raymond Ng, UBC computer science professor and Canada Research Chair in Data Science and Analytics
Developing AI responsibly
Dr. Ng understands concerns around privacy and automated decision-making in health care. He has concerns himself over developers capitalizing on AI with quickly produced tools. “They are not necessarily thinking about the best interests of the patient.”
He likens developing AI tools to creating a super-fast car engine. “With this engine, we could take patients from one place to another much faster and more efficiently.” However, he cautions, faster could translate to dangerous if the engine isn’t developed to work with the rest of the car’s systems and the needs of drivers and passengers—health care professionals and patients.
That’s why UBC researchers such as Dr. Ng are ideally positioned to help advance AI innovation in health care. “Our work at the Data Science Institute has a strong partnership with BC Provincial Health Services Authority (PHSA),” he explains. The PHSA and other organizations like BC Cancer know UBC will approach data and research responsibly to build a proof of concept.
Working with health authorities allows ongoing consultation with staff who would use the AI tools. “One of the reasons we’re so successful is that from day one, we’ve co-designed with front-line workers,” he explains. “The whole goal is to help people do their jobs much more efficiently. It’s about helping people have more time to do more important things that an algorithm cannot do well.”
The work is interdisciplinary, requiring broad expertise. “UBC has all the right people on campus to form the right teams,” he says. Faculty of Medicine graduate students Christy Kwok and Jaimie Lee collaborated on research using NLP to interpret clinical documents, such as pathology and CT imaging reports.
The team’s work has attracted interest from other health-care systems as well. Pilot projects using the technology are now being developed in the Maritimes.
Potential for individualized, user-generated care
Dr. Ng also sees the potential for NLP tools to help individuals better monitor their own health. If they choose, they could share that information with health-care providers to help monitor their conditions.
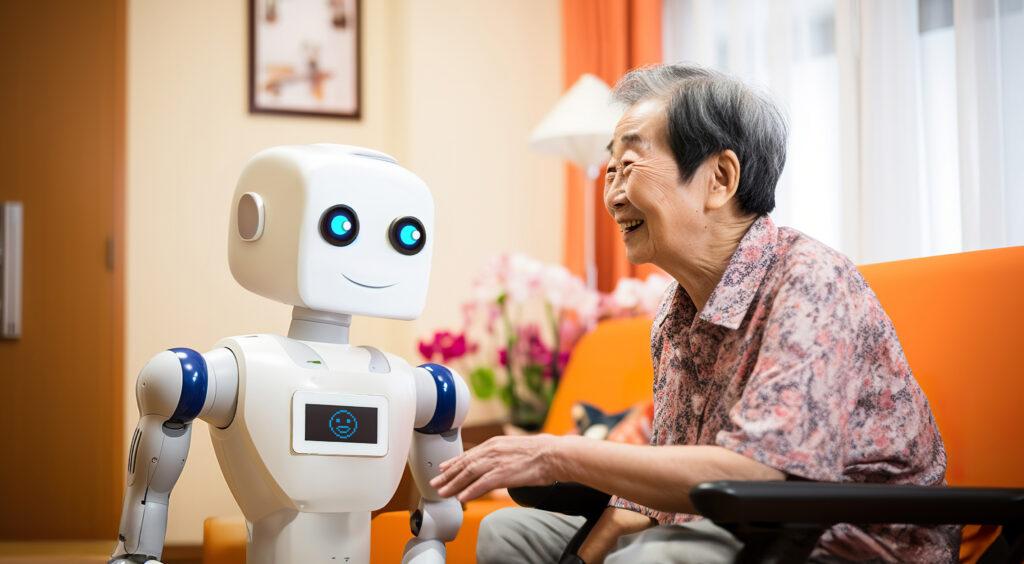
“I would love to see a system where the clinicians and the health-care systems are in constant touch with the patients,” he says. For example, isolated seniors or people with chronic illness could use text messaging, voice recordings or chat bots to report changes in sleep, mood or other conditions. “The system could monitor your well-being, and if you are really doing poorly, they will fast track you.”
When you arrive at your appointment, “all that data has already been summarized, so the doctor already knows what has happened for the past few months.”
Dr. Ng’s team is researching these possibilities and more. “There is no question that AI offers a lot of opportunities,” he says. “There’s also no question that AI can be used irresponsibly. But the technology is there and our job as leaders in this area is to put it to good use.”